
Rajaram Sharma
Assistant professor, Radio-diagnosis Pacific Institute of Medical Sciences (PIMS), Umarda, Udaipur, Rajasthan, India-313001
*Corresponding author: Rajaram Sharma, Assistant professor, Radio-diagnosis Pacific Institute of Medical Sciences (PIMS), Umarda, Udaipur, Rajasthan, India.
Received date: June 21, 2022
Accepted date: August 05, 2022
published date: September 27, 2022
Citation: Rajaram Sharma. (2022) “Mirizzi’s Syndrome: Revisiting the Findings on MRCP”, J of Gastroenterology and Hepatology Research, 3(3); DOI: http;//doi.org/09.2022/2.10135
Copyright: © 2022 Rajaram Sharma. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly Cited.
I/we certify that I/we have participated sufficiently in the intellectual content, conception and design of this work or the analysis and interpretation of the data (when applicable), as well as the writing of the manuscript, to take public responsibility for it and have agreed to have my/our name listed as a contributor. I/we believe the manuscript represents valid work. Neither this manuscript nor one with substantially similar content under my/our authorship has been published or is being considered for publication elsewhere, except as described in the covering letter
Introduction
I/we certify that I/we have participated sufficiently in the intellectual content, conception and design of this work or the analysis and interpretation of the data (when applicable), as well as the writing of the manuscript, to take public responsibility for it and have agreed to have my/our name listed as a contributor. I/we believe the manuscript represents valid work. Neither this manuscript nor one with substantially similar content under my/our authorship has been published or is being considered for publication elsewhere, except as described in the covering letter. I/we certify that all the data collected during the study is presented in this manuscript and no data from the study has been or will be published separately. I/we attest that, if requested by the editors, I/we will provide the data/information or will cooperate fully in obtaining and providing the data/information on which the manuscript is based, for examination by the editors or their assignees. Financial interests, direct or indirect, that exist or may be perceived to exist for individual contributors in connection with the content of this paper have been disclosed in the cover letter. Sources of outside support of the project are named in the cover letter.
I/We hereby transfer(s), assign(s), or otherwise convey(s) all copyright ownership, including any and all rights incidental thereto, exclusively to this journal, in the event that such work is published by the journal. The journal shall own the work, including 1) copyright; 2) the right to grant permission to republish the article in whole or in part, with or without fee; 3) the right to produce preprints or reprints and translate into languages other than English for sale or free distribution; and 4) the right to republish the work in a collection of articles in any other mechanical or electronic format.
We give the rights to the corresponding author to make necessary changes as per the request of the journal, do the rest of the correspondence on our behalf and he/she will act as the guarantor for the manuscript on our behalf.
All persons who have made substantial contributions to the work reported in the manuscript, but who are not contributors, are named in the Acknowledgment and have given me/us their written permission to be named. If I/we do not include an Acknowledgment, that means I/we have not received substantial contributions from non-contributors, and no contributor has been omitted.
|
30/07/2022 |
|
|
30/07/2022 |
|
|
30/07/2022 |
|
|
30/07/2022 |
|
Description:
Mirizzi’s syndrome is an uncommon entity that is defined as common hepatic duct (CHD) obstruction caused by extrinsic compression from an impacted stone in the cystic duct or in the gallbladder neck. [1-2] This syndrome occurs in 0.05 to 4% of patients with gallstones. [3] Approximately 50 to 70% of patients with Mirizzi’s syndrome are women because of the higher incidence of gallstones. The gallbladder is connected to the cystic duct by its neck portion, which drains into the common bile duct (CBD). Sometimes large gallstones can become impacted in the neck of the gall bladder or in the cystic duct. These gall stones cause common hepatic duct obstruction and secondary duct inflammation, leading to frequent episodes of cholangitis. Rarely, chronic inflammation may cause bile duct wall necrosis and erosion leading to chole-cystobiliary fistula. [4] Patients with Mirizzi’s syndrome may present with right upper quadrant pain, fever and jaundice. Classical Magnetic resonance cholangiopancreatography (MRCP) findings show a largely impacted gallstone in the gallbladder neck or in the cystic duct, inflamed hydropic gallbladder causing proximal dilatation of the extra and intrahepatic biliary tree. Csendes et al. classification is useful for surgical planning. Type I is extrinsic compression in the common hepatic duct by impacted stone in the neck or cystic duct or absence of cystic duct, Type II is Cholecystocholedocal biliary fistula (CCBF) involving a one- third of the CHD wall circumference, type III is CCBF with over two-thirds of the CHD wall circumference, type IV is CCBF involving the whole CHD wall circumference and type V describes any of above with a cholecystoenteric fistula.
Definite treatment of Mirizzi’s syndrome is cholecystectomy, and in the case of fistula, hepato- jejunostomy or duodenostomy can be done.
A 33-year old male presented to our institute with complaints of pain in the right upper quadrant region with 2-3 episodes of vomiting and fever. On clinical examination, the patient had yellowish discolouration of skin and eyes. The patient was advised for ultrasonography (USG) of the abdomen and routine blood investigations. The USG revealed a large impacted stone in the gall bladder with wall oedema and mild intrahepatic biliary radicles dilatation. On blood investigations, bilirubin was increased (direct bilirubin 6.5 mg/dl, total bilirubin 8.5 mg/dl), and alkaline phosphatase level was increased to100 U/L. After that, the patient was advised for MRCP to evaluate for CBD, which couldn’t be assessed on USG due to obscuration by bowel gases. MRCP depicted a large hypointense filling defect at the neck of the gall bladder representing a calculus. It was causing obstruction to the normal pathway of biliary drainage, making the gall bladder over distended. [Figure.1]The calculus was compressing the common hepatic duct near the hilum with dilatation of intra and extra biliary radicals.[Figure 2] Thus, a diagnosis of type I Mirizzi’s syndrome was made, and the intra-operative appearances were compatible with imaging findings(cholecystectomy). The patient recovered well after the surgery and doing fine.
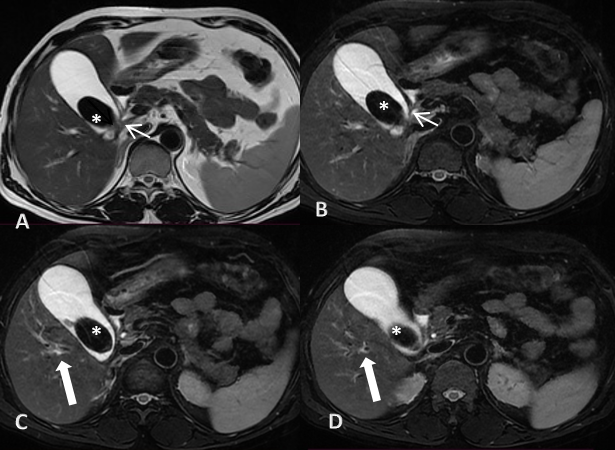
Figure 1: (A and B) axial t2w sections from MRCP abdomen, demonstrating a hypointense filling defect in the gall bladder suggestive of calculus (asterisk). There is compression of the proximal CBD (white arrows) by the calculus.
(C and D) axial t2w sections from MRCP abdomen reveals dilated intra-hepatic biliary ducts (thick white arrows).
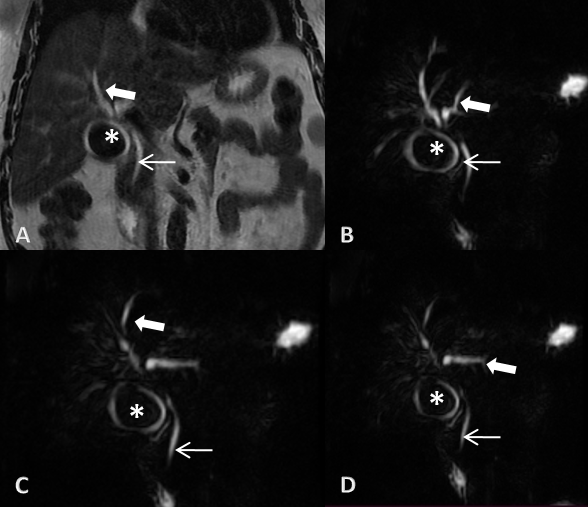
Figure 2: Coronal sections of T2W (A) and reformatted 3D MRCP (B, C and D) of abdomen showing hypointense filling defect suggestive of calculus (asterisk). There is non-visualization of compressed proximal segment of CBD with dilatation of IHBR (thick white arrows) and normal calibre distal CBD (white arrows) respectively.
Learning Points/Take Home Messages (2-3 bullet points)